1. How to minmise anaesthetic death in an old dog
Informed consent
History and physical examination
Blood test, ECG and X-rays
Sedation dosage 50% for dogs over 5 years old or not as healthy
Antidote to sedation
Emergency drugs
IV drip, antibiotics and diuretic
Intubation
Duration of anaesthesia
Close monitoring of anaesthesia by experienced assistant
Duration of surgery
Antidote
Recovery. Not to go home immediately
Post op antibiotics and painkillers for extracted teeth
Oct 28, 2014. A father and young adult daughter presented this gentle 7-year-old male Sheltie for dental scaling. A friend's Maltese had died after dental scaling by another vet and so the owners were worried about anaesthetic death. "Dogs usually do not die under anaesthesia or after anaesthesia," I said to the father. "Unless the dog has heart disease or poor health."
A thorough physical examination showed that this Sheltie with bad breath was generally healthy in heart and lungs. The heart beats were irregular. 50% sedation of domitor and ketamine IV calmed this nervous Sheltie.
Health screening including a complete cell count and X-rays of the chest is advised. No ECG is done.
In this case, I gave an IV drip, with IV baytril, frusemide and Vit B complex.
It is very important to provide a very close monitoring of the maintenance of isoflurane gas at 0-2%, oxygen flow rate at 2 litres/minute to ensure that minimal anaesthesia is being given. The dog did wake up in the midst of dental scaling as the maintenance dose was 0.5%.
He was intubated again and maintained at 2%. The dog woke up fast and went home 3 hours later. Follow up 2 days later showed that the dog is OK. The dog had been given dry dog food and milk since young. He likes only certain brands of milk. Well beloved family dog and in excellent body condition.
FOLLOW UP
Oct 28, 2014
A new client - father and young adult daughter brought in a 7-year-old male entire Shetland for dental scaling. Their friend's Maltese had died after dental scaling in another vet practice and so they did not want to go to the practice.
"Very rarely do dogs die after waking up from anaesthesia given for dental scaling," I said. "Was the Maltese having heart diseases?" The owners of the gentle full sized Sheltie did not know but they would avoid this friend's vet
No vet can guarantee no anaesthetic risk. Even people do die.
PHYSICAL EXAMINATION
Other than periodontal disease grade 4 (tissue attachment loss over 50%), I noted that this Sheltie had congested maroon red gums, not the normal pink ones. You can see this in the video. Why? The capillary refill time was longer than the usual 2 seconds. Blood test showed that this dog had a higher than normal amount of haemoglobin in his blood at
19.1 (12-18). The total red cell count was normal. The haematocrit was normal too. Platelets were normal. What does it mean? Was he fed some supplements?
BLOOD TEST on 27.10.14 Abnormal values
Urea 12.3 (4.2 - 6.3)
Creatiine 65 (89-177)
Haemoglobin
19.1 (12-18)
All the other blood values within normal limits.
FOLLOW UP - Day 2 after dental scaling
The dog was a bit tired yesterday but is Ok and eating today.
"Tartar started to build up fast in last 3 years," the father said that the dog was not given meat. "Could it be the milk making the kibbles soft?". This dog had the biggest crusty tartar I had ever seen in a dog (see image/video).
The dry dog food was Science Diet Lamb and Rice with a brand of dog's milk since young. Dog treats were given.
ADVICES 2 DAYS LATER
No milk and treats to prevent tartar build up.
Eat dry food without milk and drink water.
Blood test 4 weeks later to check on the urea levels.
This case shows that a blood test is important for screening the health of an older dog. The owner was given the option. The blood test was done by me as this dog had an unusual congested gums.
-------------------------------------------------------------------------------------------------------
DENTAL WORK WITHOUT ANAESTHESIA IN A VERY OLD POMERANIAN WITH HEART DISEASES Dr Sing Kong Yuen, BVMS (Glasgow), MRCVS
Written: 04 September, 2010 |  toapayohvets.com toapayohvets.com
Be Kind To Pets
Veterinary Education
Project 2010-0129 |
Can an old vet (>50 years old) change his mindset of not using general anaesthesia and sedation for very old dogs so that she has a high probability of being alive at the end of dental work? The only chances of her dying would be from fright (heart failure) due to the stress of the dental work without general anaesthesia. Seldom are such old dogs healthy. They usually have heart disease and general anaesthesia kills them as they are also very old.
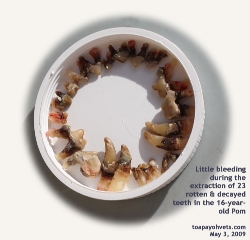
Is it possible to perform dental extraction with no general anaesthesia for such very old dogs with heart diseases and a mouthful of decayed and rotten teeth as shown in the pictures of a case of a 16-year-old Pomeranian below? |
 |  |
| 16-year-old. Home cooked food. Teeth encrusted with tartar but surprisingly there was no strong bad breath smell. | An I/V glucose drip is important for aged dogs during operation. Emergency Lasix was given I/V when the dog coughed trying to clear her throat. |
 | 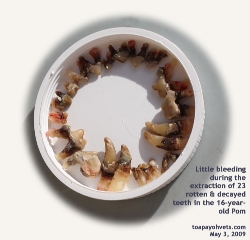 |
| Dog goes home with no teeth left. Vet Intern Ms Toh arranged the teeth neatly for photography. "How many teeth has an adult dog?" I tested Ms Toh who had great interest to study veterinary medicine. She shook her head. The answer is 42. |
If she survived, her quality of life (no daily oral pain and infection and hence able to enjoy her food and put on weight). She would be more active and alert. She might live to a ripe old age the bacteria in her mouth had been rid of.
Bacteria constantly produce toxins and lower her immune system. In the above case, the Pomeranian was in good condition for her age. She looked like an 8-year-old dog rather than an ancient canine. She had no fever and no abnormal respiratory rate. The pulse pressure was lower. The dog was on heart medication prescribed by Vet 1 for some years. However, she was underweight. Her mouth was not smelly despite the presence of large amounts of tartar.
The owner requested "manual scaling" as she had discovered in the internet forum that I was highly recommended as I do "manual scaling" (without general anaesthesia). "I don't do manual scaling," I told her that there was a mistake in the internet forum she had researched. "How many manual scaling in dogs have you performed?" she asked. "None," I said. Ultrasonic dental scaling is the method I use.
However, this old dog needed dental extraction and not dental scaling. The roots of the teeth were all loose and infected. "Manual scaling" (without general anaesthesia) would not be in the interest of this dog as the bacteria still would be multiplying under the roots below the gums. Dental scaling would be what the lady wanted but this was not the right thing to do for the dog.
"There is a risk that your old dog may die from fright due to the pain of tooth extraction without general anaesthesia," I informed the lady. She was surprised and said, "Let me have some time to think as to what to do."
I expected the lady to go home on this sunny Sunday afternoon of May 3, 2009. I had my hands full on this busy Sunday. However, she returned and decided to take the risk.
THE PROCEDURE
An I/V glucose drip was given to help to increase the blood pressure as the pulse was weak. Into the drip set, I gave Baytril antibiotic to reach the dog immediately to kill the bacteria.
The dog was quite docile and so there was not much worry. Two front incisor teeth were extracted. The dog started coughing as if to clear phlegm in her throat. This indicated that the oral heart medication given to the dog was not effective to remove the fluid in the lungs (pulmonary edema). What now? Cease operation?
Going back to the basic of veterinary pharmacology, I needed a drug to clear the water from the lungs quickly. I broke a vial of Lasix and injected it into the IV drip. The drug would take away fluid from clogging the airways by taking it into the blood-stream. I waited 5 minutes before continuing dental extraction.
One or two teeth were extracted at 1-2-minute intervals. The teeth were so loose that most of them could just be pulled out easily. There was little bleeding. Tissues were used to control the bleeding. When the bleeding had stopped, the other teeth were extracted.
The dog had not even coughed throughout the process of dental extraction. He was apprehensive. Suddenly the dog shifted and the IV catheter came out. Intern Ms Toh had informed me that there was a skin swelling above the catheter. 3 Elastoplasts strips and a wrap-around bandaged had been used to fix the catheter in place but we had anticipated that this would happen. The dog had around 100 ml of glucose and that would be sufficient. Since the catheter had popped out of the vein, the rest of the fluid was given subcutaneously. Caution would be the key and there was rest in between each dental extraction, dragging the process to over one hour. Prevention of heart failure due to fright was paramount. After all, the owner wanted an effective veterinarian who would produce a live dog at the end of the day, not an efficient one with a dead body.
CONCLUSION
The dog had 23 loose and rotten teeth extracted with little pain and little bleeding. The lady's eyes brightened when she returned later and was told that her dog was OK. The dog was alert and her excellent coat shone golden in the evening rays of the evening sun as I took her photograph. As the dog was not vaccinated, I did not want the dog to be hanging around the Surgery. The lady put the dog in her car while she paid the bill. Well, the dog peed inside her car, but she was not upset. Her best friend was alive and that was what mattered to her.
This is the sole case of me doing dental work without general anaesthesia in my 2 decades of small animal practice. I record this in detail to share my unusual experiences with other veterinarians. If the dog had kicked the bucket, the owner would be very unhappy as she had 14 years of companionship with this old friend after adoption from the SPCA as a 2-year-old.
It was fortunate that the old Pomeranian did not die of fright on the operating table. I don't want to do any more such cases as this will tempt the God Of Death. This was not a simple case as the dog was coughing. If the coughing continued, the dog was be stressed out and die of heart failure. Therefore, the vet must know what to do when things don't proceed smoothly. Of course, the best way is not to accept such a high-risk case as deaths of companion animals on the operating table are never forgiven or forgotten by the owner and her family.
NOTE:
It would be wise for dog owners to get the dog's teeth check every year and get dental scaling done when the dog is young and fit. Continue with tooth brushing after dental scaling.
UPDATE IN SEP 4, 2010 FROM OWNER:The dog lived to a ripe old age and passed away in April 2010. The post-operation feedback from the owner indicated that the dog had oral pain and low blood sugar.
| E-mail to Dr Sing dated Sep 2, 2010 | |
bekindtopets.com/dogs/20080828Dog_Dental_Problems
_Singapore_ToaPayohVets.htm
Dear Judy,
I saw the case study on the above website.
I am the owner of this dog. Her name is She. She passed away this year 11 April. It was a Sunday morning.
Please send my regards to Dr Sing.
On the case study, I would also like to update you what happened after I got home.
The surgery was a success as my dog was indeed alive and well. Just like any other beings, they need rest after surgery.
However dogs will always attempt to walk or run as its part of their nature, not knowing itÂ’s exhausting.
One the first night after the surgery, my dog collapsed suddenly and started to whine. I picked her up and gave her a massage, which she was able to stand on her feet soon after. This happened for another 2 times in a day.
I realized it may be trauma and shock, and maybe low glucose level. She is also not eating well. Where is she going to get the “energy”?
She was already on long term medication for heart, plus after surgery medicine. I was not prepared for more medication for my little 16+ yr old.
I brought her to TCM. I think this doctor is the only doctor in SG who provides acupuncture for dogs. He is (Name given). I asked this doctor to also do treatment for her appetite, her heart, and other senses such as hearing and sight. She responded very well after the first treatment. She was also beginning to eat! And best part is she and I had eye contact, it shows that sheÂ’s getting more alert.
She continued the treatment for about 1 month, about 5 consultations. She recovered very well. Soon after she starts to bite all people who attempt to touch her, including myself. I think itÂ’s the surgery trauma and old age crankiness. But I also think that if she bites it means she is alert to her surroundings. I see it as something positive, sometimes, funny.
Because, no teeth still want to bite people?
No more bad breathe and no more toothache. I was not worried about bacteria possibly worsening her heart condition anymore.
Without teeth, her tongue always sticks out! Amazingly she looked even younger and cuter!
I wrote this to you because as fate has it, Dr Sing has indeed changed the quality of her life.
But he is also right, itÂ’s very risky. What if the owner did not take precaution AFTER the surgery?
I have attached 4 pictures. 1 taken in May 2009, 1 in Sep 2009 and 1 less than a month before she left in 2010.
She was very lucky, to have met the right people.
Thank you.
Best Regards,
|
| E-mail from Dr Sing dated Sep 4, 2010 | |
I am Dr Sing and got your good news of your dog living to a ripe old age. Thank you for your email and important feedback post-operation as I seldom get any feedback. Most likely it was low blood sugar as you diagnosed. It could be the post-dental extraction pain. Your pictures are great. Pl give permission to post the pictures. I hope all are well with you.
|
| E-mail to Dr Sing dated Sep 4, 2010 | |
Hi Dr Sing,
Great to hear from you!
Sorry I would like to rephrase, I meant her fear and anxiety on the surgery table would definitely caused that “weakness” which makes her faintish.
Yes, I should write as low blood sugar. ItÂ’s a normal after-surgery process. I remember feeding her sugar/glucose water.
I am well, thank you. I guess this is one thing all dog owners have to go thru.
Until yesterday, I could never have imagined how hard you guys work over the metal table, while I was stoning in your clinic.
It was a very detailed re-enactment. Thank you for sharing. It was heartwarming for me.
I hope my feedback could help you and your furry patients.
Please feel free to use the pictures, itÂ’s my pleasure.
|
 TIPS FOR VETS: TIPS FOR VETS:
POST-OPERATION PAINKILLERS
I did not give the dog pre-op NSAID pain-killer nor after the dental extraction as I would do for a younger dog. This is because this dog's kidneys would not be as good as a younger dog to withstand any adverse reactions on the kidneys from NSAID drugs.
NSAID drugs are not to be given to dogs with kidney disorders and though no blood tests to ascertain renal function were taken, I expected the kidneys and livers of a 16-year-old dog not to be as normal as to metabolise NSAID drugs without dying of side effects and thereby distressing the lady owner. As for post-operation sugar paste, this would be given for old dogs. In very old dogs, it is very risky to use injectable anaesthesia. In this case, isoflurane gas would be safer but it was not used as the owner |
|
|
|
 toapayohvets.com
toapayohvets.com